When the Body Knows

The Cucumber, the Vine, and Ripeness
The wisdom found me a week later.
I’m standing in the corridor outside the ICU, discussing with my residents about Mrs. Shantha. Eighty-two, chronic lung disease, pulmonary hypertension, end-stage heart failure, fourth admission this year. Each time a little weaker. This time her kidneys are failing too.
Her son appears beside me. “Doctor, we want everything done. CPR if needed. Ventilator. Whatever it takes.”
But her body was saying what her family can’t hear yet.
“Can I be honest with you?” I ask.
He nods, but I see the fear in his eyes.
“Your mother’s body is not doing well. Not her mind… she’s alert, she’s there. But her heart can’t pump anymore. Her kidneys aren’t working too. We can support these functions with medicines and machines for a while. But we’re not reversing anything. We’re just… holding on.”
“So we should let her die?” Defensive. Angry.
God, I don’t like how this sounds. Like I’m giving up. Like I don’t care.
“No. I’m saying we should ask… what does she want? Not what we want. What would she choose if she fully understood what ‘doing everything’ actually means?”
We talk. Really talk. An hour. I explain what CPR looks like in an 82-year-old with brittle bones. What a ventilator means long-term. What dialysis involves. The days in ICU. The loss of independence. The probability of meaningful recovery.
He finally says, “Can I ask her?”
“Yes. Please.”
They have the conversation that afternoon. Just the two of them. Inside the ICU. I don’t know what was said. But when he finds me later, his eyes are red but his shoulders are lighter.
“She said she’s tired. She said she’s lived fully. She wants to be comfortable, wants to go home if possible, doesn’t want machines.”
We shift to comfort care. Optimize her heart medications for symptom control, not survival. Manage her breathlessness. Two days later, she goes home with oxygen arranged at home for support.
She dies six days after that. In her own bed. Her children and grandchildren around her. No CPR. No tubes. Just morphine for comfort and the Hanuman Chalisa playing softly.
Her son calls me after the funeral. “Doctor, thank you for asking the right question. She was ready. We just needed permission to see it.”
She was ready.
That’s the word that stays with me.
Not “dying” or “failing” or “giving up.”
Ready.
But I’ve also pushed back the other way. When readiness wasn’t there yet.
Mr. Shekhar, 84, had a massive heart attack. His wife wanted to withdraw life support on the third day. “He’s suffered enough, Doctor” she said, crying. “Let him go.”
I looked at his numbers. Bad… yes. But his heart was still responding to medications. His kidneys, though stressed, were still producing urine. His lungs were showing some improvement on the ventilator.
“I understand he’s suffering,” I said gently. “But his body is still fighting. Still responding. Some parameters are better today. He’s exhausted, not finished. Can we give him a few days?”
She agreed.
He was discharged from the hospital 15 days later. Started going for a walk in two months.
So what’s the difference between Mrs. Shantha and Mr. Shekhar?
Not age… she was 2 years younger. Not severity… both were critical. Not even diagnosis… both had failing organs.
Something else. Something I was learning to sense but couldn’t quite name.
Until the teaching came.
An elderly man approaches me when I’m visiting a temple a few days later. I recognize him. He was one of the family elders from Kumar’s 13th-day ceremony.
He holds my hand with both hands. “Doctor, you helped the youngsters in our family understand when to let go. I wanted to share something with you. Something that helped me forty years ago when my father died.”
He hands me a small book. Sanskrit verses with translations. Opens to a specific page.
“This is what I whisper when I’m afraid. When death is near. For myself or for those I love.”
I see the verse. The Maha Mrityunjaya Mantra.1 I know it. But he points to one specific line:
“urvārukamiva bandhanān mṛtyormukṣīya mā’mṛtāt”
“Liberate me from death, just as a ripe cucumber separates from its vine.”
I look at him, confused. A cucumber?
He smiles. “Come. Let me show you something.”
We walk to a small garden behind the temple. There’s a small garden of flowers and some vegetables. Cucumber vines climbing a metal grid.
He points to a small, green cucumber. “See this one? Young. Still growing. Watch.”
He tries to pluck it. The connection is strong. The cucumber resists. He’d have to twist it, pull it, and use force.
“Violence,” he says quietly.
Then he points to another cucumber. Larger. Golden-yellow. Fully formed.
“This one? Ripe.”
He barely touches it. The cucumber drops into his hand. The stem connection had already weakened. Natural. Effortless.
He hands me the ripe cucumber. “We’re not praying to live forever, Doctor. We’re praying to live fully… to ripen with experience and wisdom and completion. And when that ripeness comes, when our time is complete, we pray we won’t cling to the vine. We’ll simply… drop.”
Anayasena. Without struggle.
I stood there holding that cucumber, and something clicked.
Mr. Shekhar was the green cucumber. Still growing. Still forming. His body was exhausted but not complete. He had more life to live. More capacity to recover. Plucking him from the vine on day three would have been violence.
Mrs. Shantha was the ripe cucumber. Full. Complete. Ready. Her body had done its work. She’d lived fully, loved deeply, raised children, seen grandchildren. The connection to life was naturally weakening. She knew it. We didn’t need to hold on to her with machines. We just needed to… let her drop.
The ancient prayer wasn’t about giving up. It was about recognizing ripeness.
I started seeing it everywhere.
Mr. Charles, 68, sudden brain hemorrhage. Devastating. But fit. Previously healthy. Body fighting hard. Not ripe.
We pushed through two weeks of touch-and-go. Ventilator. Dialysis. The whole arsenal. His wife asked me daily, “Is there hope?”
“His body is still responding,” I told her. “Still fighting. Let’s give him time.”
He survived. Rehabilitation took a long time. But he walked again. Talked again. Returned to a different life, yes, but a life.
Mrs. Fatima, 69, similar hemorrhage. But multiple previous strokes. Weak baseline. Frail. Body saying “enough” in every measurable way.
I sat with her family. “Her brain damage is extensive. But beyond that, her body has been struggling for years. Heart disease. Diabetes. Previous strokes. She’s unlikely to make it.”
They understood. We offered comfort care. She died peacefully two days later, her daughter holding her hand, softly singing a hymn she’d loved.
Both had brain hemorrhages. Both had families struggling with the decision. But one was green, one was ripe.
And learning to tell the difference became my most important clinical skill self-training.
It’s not purely objective. Two patients with identical diagnoses can have completely different levels of ripeness.
It’s a combination of:
- How their body responds to treatment
- What their baseline was before this illness
- What they’ve lived through already
- What they still want to live for
- How their own spirit relates to their body
Sometimes I sense it in the way they look at me. A certain peace in the eyes. An acceptance.
Sometimes I sense it in the family. They’re not ready to let go, but the patient is.
Sometimes I sense it in the body’s response. We’re giving everything possible, and it’s just… not accepting. Not responding. The body as a whole is shutting down despite our best efforts to support individual organs.
The rituals started making more sense too.
I attended another patient’s ceremonies a few months later. This time I discussed with the priest.
The priest explained to me quietly, “Each day, we symbolically release one more connection. The body. The senses. The relationships. Not in grief alone… in honour. We’re not forgetting. We’re transforming our relationship from physical to spiritual.”
Day one is raw. The family can barely function. The rituals force them to gather, to cook specific foods, to chant specific prayers. Follow a structure when everything feels chaotic.
By day seven, something shifts. The crying is less constant. They can talk about the person with smiles, not just tears.
By day thirteen, they’re ready. Not healed… grief doesn’t work that fast. But ready to begin moving forward.
It’s a decompression process. You can’t rush it. You can’t skip steps.
The ancient seers understood what modern grief counseling is only now rediscovering… grief needs time, structure, and community. You can’t process loss in isolation. You can’t rush it with medications or therapy shortcuts. You have to sit with it, surrounded by ritual and loved ones, until it changes from unbearable to bearable.
I remember standing at Nagesh’s ceremony two years ago, not understanding what I was witnessing. Just feeling the weight of loss.
Now I see it differently.
The ceremony wasn’t about him. He’d already dropped from the vine. Ripe. Complete.
The ceremony was for us. The ones still attached. Still holding on.
Thirteen days to practice our own letting go. To loosen our grip on the physical form we’d known. To accept that the person we loved hadn’t ended… just changed clothes, as the Gita says.
Vasamsi jirnani yatha vihaya.2
The soul discards worn-out bodies like worn-out clothes.
Nagesh’s body had worn out. Liver disease, slow and exhausting. By the end, the body was just a painful vessel. He was ready to discard it.
The ceremony helped us see that. Accept that. Honour that.
But how do you know ripeness before the person dies? That’s the clinical question. Critical question.
I’m learning. Slowly.
It’s not in the textbooks. It’s not a lab value or a scan finding.
It’s something you develop after spending enough time at the bedside. After enough conversations. After enough moments of pushing when you should have released, and releasing when you should have pushed.
It’s pattern recognition, yes. But deeper than that.
The body knows when it’s done. It signals in a hundred small ways:
- Progressive failure despite maximum support
- The patient’s own words: “I’m tired, Doctor”
- The look in their eyes when you ask if they have any pain or difficulty
And sometimes, the patient tells you directly.
“Doctor, I’ve had enough. I want to go home.”
Sometimes, they are even more direct.
“Doctor, I’ve had enough. I want to die.”
When someone says that… clearly, repeatedly, with full understanding… they’re telling you they’re ripe. Ready to drop.
Our job isn’t to argue. Our job is to honour it. Discuss about it.
I think about Mrs. Shantha. She didn’t use the word “ripe.” She said “tired.” But it meant the same thing.
I think about Mr. Shekhar. His body wasn’t ready. And his wife’s exhaustion…understandable as it was… didn’t change that.
I think about the green cucumber. The ripe cucumber.
The violence of premature plucking. The grace of natural separation.
Standing in that temple garden, holding the cucumber the elder had given me, I finally understood what I’d been searching for at Kumar’s ceremony.
The difference between fighting death and accepting it isn’t about giving up or pushing harder.
It’s about recognizing the season.
Green cucumbers need time, support, nourishment. They’re still becoming.
Ripe cucumbers need permission to drop. They’ve already become.
Both deserve our full attention. Our full care. Our full respect.
But they need different things from us.
I’m learning to ask: Which season is this patient in?
Still ripening? Then my job is aggressive support. Bridge them through this crisis. Give them time to recover, to complete, to ripen fully sometime in the future.
Already ripe? Then my job is different. Not prolonging. Not delaying. But honouring. Comforting. Allowing the natural separation without violence. After a family discussion.
The hardest part? I don’t always know. Even now.
Sometimes I get it wrong. Sometimes I push when I should have let go. Sometimes I let go when there was still more ripening to do.
But I’m learning to listen. To the body. To the patient. To that quiet voice inside that whispers: Ready. Not ready.
The elder who taught me this gave me one more gift before he left.
He opened the small book again. To another prayer.
“This one,” he said, “is specifically for physicians. For people like you who stand between life and death every day.”
I read it:
Anayasena maranam,
Vina dainyena jeevanam.3
Death without struggle.
Life without indignity.
“That’s the prayer I needed,” I said quietly.
He nodded. “It’s the prayer we all need. But especially those who witness both every day.”
“Anayasena” Series
This article is part of the six-part series that explores what modern medicine can learn from ancient wisdom about dying well, living with dignity, and letting go with grace.
Subscribe to get an email when the other articles are published.
- How Do I Know I’m Right? The weight of end-of-life decisions
- When the Body Knows. The cucumber, the vine, and ripeness
- The Prayer I Whisper. Anayasena Maranam and dignity in dying
- What the World Taught Me. Ancient wisdom across cultures
- The Conversation Nobody Wants to Have. Guidance for families facing end-of-life decisions
- The Weight Doctors Carry. The practice physicians need for end-of-life care
Author’s note
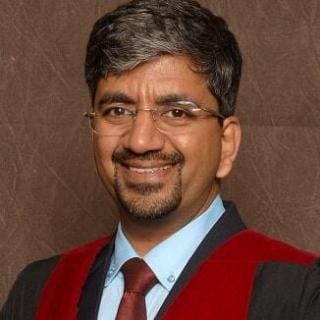
Dr. Shashikiran Umakanth (MBBS, MD, FRCP Edin.) is the Professor & Head of Internal Medicine at Dr. TMA Pai Hospital, Udupi, under the Manipal Academy of Higher Education (MAHE). While he has contributed to nearly 100 scientific publications in the academic world, he writes on MEDiscuss out of a passion to simplify complex medical science for public awareness.